How does the new coronavirus compare with the flu?
Содержание:
- Symptoms
- Тяжелая форма коронавируса
- Why has WHO declared a global emergency?
- Death rate
- Allergies have chronic symptoms
- Как проявляется коронавирус у человека
- Coronavirus Vaccine
- Symptoms and severity
- Which virus makes you sicker?
- The bottom line
- Similarities: COVID-19 and the Flu
- Myth 2: Lockdowns slow the spread
- Myth: Drinking bleach or other disinfectants can protect you from COVID-19
- Virus transmission
- The coronavirus outbreak isn’t considered a pandemic
- Myth: The virus was probably made in a lab
- Summary
- Легкая форма заболевания
- Comparing the flu and the Wuhan coronavirus
- How R0 works
- Differences: COVID-19 and the Flu
- Myth: Wearing masks can cause CO2 poisoning
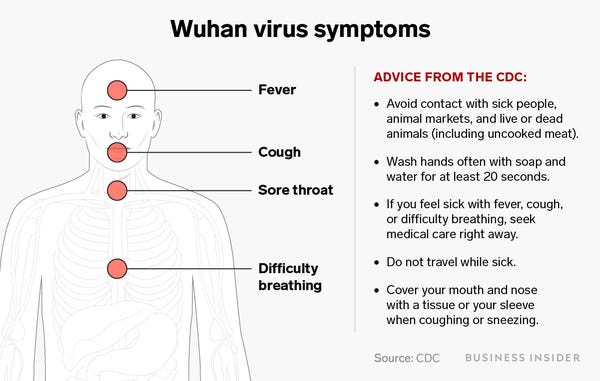
Symptoms
Both seasonal flu viruses (which include influenza A and influenza B viruses) and COVID-19 are contagious viruses that cause respiratory illness.
According to the CDC, the flu typically manifests itself in symptoms such as fever, cough, sore throat, muscle aches, headaches, runny or stuffy nose, fatigue and, occasionally, vomiting and diarrhea—typically, the latter two are more common in children. Those flu symptoms often come on suddenly after an incubation period of two to five days.
While the majority of people infected with the flu will be fully recovered in about two weeks, for some people (most often those with compromised immune systems), the flu can lead to complications like pneumonia. According to recent data from the CDC, this year just 1% of people suffering from the flu have been hospitalized.
As for COVID-19, the CDC describes a wide range of symptoms, such as fever; cough; shortness of breath or difficulty breathing; chills or shaking with chills; muscle pain; headache; sore throat; and loss of taste or smell, coming on two to 14 days after exposure to the virus. One study, involving just 100 people with the virus, published January 30 in the The Lancet, noted that the most common symptoms were fever, cough and shortness of breath, with approximately 5% reporting sore throat and runny nose, and just 1-2% reporting diarrhea, nausea and vomiting.
If the symptoms sound extremely similar, that’s because they are, according to Manisha Juthani, MD, a Yale Medicine infectious disease specialist. “Based on symptoms alone, COVID-19 and flu are very difficult to distinguish,” says Dr. Juthani.
RELATED: Coronavirus May Be Spreading So Quickly Due to Fecal Transmission, Says New Research
Тяжелая форма коронавируса
Если COVID-19 протекает тяжело, у человека развивается пневмония. Такой сценарий заболевания более всего вероятен у тех, чей возраст 60 лет и больше, а также есть сопутствующие хронические заболевания сердечно-сосудистой и/или дыхательной системы. Проявления в этом случае следующие:
- Повышенная частота дыхания, превышающая классический параметр для взрослого (12-18 вдохов за 1 минуту), даже в состоянии покоя.
- Выраженная затрудненность дыхания.
- Человек при тяжелой форме не может произнести предложение, не прерывая его, чтобы сделать дополнительные вдохи.
- Температура тела высокая, превышает +38,5°C, часто достигает показателя +39°С и более.
- Человек не может успокоить дыхание (оно поверхностное и ускоренное) и делать вдохи-выдохи медленно и размеренно.
- При тяжелой форме наблюдают апатичность больного, привычные и интересные занятия его не увлекают, он ничего не хочет делать.
- Аппетит, как и чувство жажды, фактически отсутствует, человек не хочет есть даже любимые блюда – они могут вызывать тошноту.
- Часто при тяжелом течении коронавирусной инфекции наблюдают понижение артериального давления.
В случае подобной пневмонии способен развиться ТОРС – тяжелый острый респираторный синдром. При нем альвеолы в легких воспалены, в них скапливается жидкость, которая препятствует выполнению ими своей функции. В подобной ситуации требуется искусственная вентиляция легких при помощи специализированного аппарата, так как обычное дыхание невозможно.
Why has WHO declared a global emergency?
WHO has declared a global emergency because the coronavirus is continuing to spread to other countries.
“The main reason for this declaration is not what is happening in China but what is happening in other countries,” said WHO chief Tedros Adhanom Ghebreyesus.
He said that epidemics in Iran, Italy, South Korea and Japan were the WHO’s main concern.
In the past 24 hours there were almost nine times more coronavirus cases reported outside China than inside, but the disease can be contained with the right measures, he said.
Read more: MWC 2020: Sony becomes latest tech firm to pull out due to coronavirus
Tedros has described the virus as an “unprecedented outbreak” that has been met with an “unprecedented response” and praised the “extraordinary measures” Chinese authorities had taken.
Death rate
The death rate from seasonal flu is typically around 0.1% in the U.S., according to news reports.
Though the death rate for COVID-19 is unclear, almost all credible research suggests it is much higher than that of the seasonal flu.
It’s important to note that there is no one death rate for COVID-19; the rate can vary by location, age of person infected and the presence of underlying health conditions, Live Science previously reported.
Among reported COVID-19 cases in the U.S., nearly 6% have died. This is what’s known as the case fatality rate, which is determined by dividing the number of deaths by the total number of confirmed cases. But the case fatality rate is limited for a few reasons. First, not everyone with COVID-19 is being diagnosed with the disease — this is in part due to testing limitations in the U.S. and the fact that people who experience mild or moderate symptoms may not be eligible for or seek out testing. As the number of confirmed cases goes up, the fatality rate may decrease.
Researchers from Columbia University recently estimated that only 1 in 12 cases of COVID-19 in the U.S. are documented, which they said would translate to an infection fatality rate of about 0.6%, according to . But even this lower estimate is still at least six times higher than that of the flu. (The case fatality rate in people who become sick with flu may be 0.1%, but when you account for people who become infected with flu but never show symptoms, the death rate will be half or even a quarter of that, the Post reported.)
What’s more, unlike the flu, for which there is a vaccine, everyone in the population is theoretically susceptible to COVID-19. So while the flu affects 8% of the U.S. population every year, , between 50% and 80% of the population could be infected with COVID-19, according to a study published March 30 in the journal . In the U.S., that would translate to 1 million deaths from COVID-19 if half the population becomes infected and there are no social distancing measures or therapeutics, the Post reported.
Another limitation with the case fatality rate is that some people who are counted as confirmed cases may eventually die from the disease, which would lead to an increase in the death rate. For example, South Korea initially reported a case fatality rate of 0.6% in early March, but it later rose to 1.7% by the beginning of April, according to .
Related: Why are more men dying from COVID-19?
It’s also important to note that estimates of flu illnesses and deaths from the CDC are just that — estimates (which make certain assumptions) rather than raw numbers. (The CDC does not know the exact number of people who become sick with or die from the flu each year in the U.S. Rather, this number is estimated based on data collected on flu hospitalizations through surveillance in 13 states.) A recent paper published in the journal JAMA Internal Medicine emphasized this point when it found that, in the U.S., there were 20 times more deaths per week from COVID-19 than from the flu in the deadliest week of an average influenza season, Live Science previously reported.
Allergies have chronic symptoms
COVID-19, like the flu or common cold, is an acute illness, meaning people feel fine until symptoms start showing up.
Allergies, on the other hand, “are usually chronic, presenting with symptoms off and on for weeks, months, or even years,” Dr. David M. Cutler, family medicine physician at Providence Saint John’s Health Center in Santa Monica, California, told Healthline.
Experts also noted that, in most parts of the country, it’s not allergy season yet.
“Allergies should not cause a fever or body aches,” Arthur said. “Generally, no cough unless you have a lot of nasal drainage.”
Allergies also may cause wheezing, she added, especially in people with asthma.
“Allergy symptoms tend to vary with the environment: worsening with exposure to dust, pollen, or animal dander, whereas cold symptoms tend to persist regardless of time of day, weather, locality, or other environmental factors,” Cutler said.
Also, as with COVID-19, “Colds are more likely to have generalized symptoms like fever, headache, and body aches, whereas allergies usually affect only the respiratory tract,” Cutler said. “Allergy symptoms tend to improve with antihistamine and other allergy-specific medication. Colds are more likely to respond to decongestants, acetaminophen, fluids, and rest.”
With some schools reopening, the CDC issued new guidelines in mid-August on the differences in symptoms between COVID-19 and seasonal allergies.
The agency noted that things such as shortness of breath, coughing, fatigue, headache, and sore throat can be symptoms of either COVID-19 or allergies.
Itchy eyes and sneezing are generally only symptoms of allergies.
Fever, muscle aches, a loss of taste or smell, nausea, and diarrhea are associated with COVID-19 and not allergies.
The CDC recommends that all people wear cloth face masks in public places where it’s difficult to maintain a 6-foot distance from others. This will help slow the spread of the virus from people without symptoms or people who do not know they have contracted the virus. Cloth face masks should be worn while continuing to practice physical distancing. Instructions for making masks at home can be found here. Note: It’s critical to reserve surgical masks and N95 respirators for healthcare workers.
Как проявляется коронавирус у человека
У многих взрослых и детей коронавирус протекает как простуда или грипп, но самочувствие при этом несколько хуже. То есть – у приблизительно 80% заболевших COVID-19 наблюдают в легкой форме. В этом случае какой-либо специфической терапии врачи не назначают, а проводят симптоматическое лечение, выписывая препараты исходя из жалоб своих пациентов. Но приблизительно 1 из 6 заболевших переносит коронавирусную инфекцию в тяжелой форме – с развитием дыхательной недостаточности. Если человек в преклонном возрасте, при этом у него есть хронические болезни сердечно-сосудистой, дыхательной систем или диабет, вероятность тяжелого течения COVID-19 у него повышается.
У взрослых
По информации ВОЗ, главные симптомы коронавируса – затрудненность дыхания, лихорадка и кашель без отделения мокроты. Также эксперты сообщают, что внезапная потеря вкуса либо обоняния потенциально указывает на COVID-19. Так, коронавирус у взрослого человека проявляется следующими симптомами:
- рост показателей температуры тела – приблизительно в 90% случаев;
- одышка – порядка 55%;
- кашель – сухой либо с небольшим количеством отделяемой мокроты – 80%;
- чувство сдавленности в груди – до 20%.
Перечисленная симптоматика актуальна для молодых людей. Редко (у менее 10% заболевших) без повышения температуры проявления коронавирусной инфекции бывают такие:
- головные боли;
- расстройство пищеварения;
- тошнота и позывы ко рвоте;
- ощущение усиленного сердцебиения;
- кровохарканье.
Подозреваете ли у себя коронавирус на данный момент?
Да, все признаки имеются 29.87%
Да, и это уже точно 10.37%
Да, но больше склоняюсь к тому, что это обычная простуда 31.29%
Нет 28.47%
Проголосовало: 3656
У детей
У детей коронавирусная инфекция также проявляется на начальном этапе повышением температуры и кашлем. Тем не менее есть и другая симптоматика:
- диарея и другие проблемы с ЖКТ;
- головные боли;
- заложенность носа;
- отсутствие обоняния либо вкуса;
- болезненность в области груди;
- боли в мышцах.
По данным наблюдений, в детском возрасте коронавирусная инфекция чаще провоцирует нарушения пищеварительной функции. Тем не менее у подавляющей части детей, у кого был выявлен COVID-19, улучшение состояния происходило уже на следующие сутки с момента возникновения первых проявлений коронавируса. Только малый процент заболевших требует специфического лечения, интенсивной терапии и искусственной вентиляции легких. В подавляющей части случаев у детей болезнь протекает в легкой форме.
Считаете ли вы, что коронавирус не так опасен, как о нем говорят?
Да 25.91%
Нет 56.36%
Затрудняюсь ответить 17.73%
Проголосовало: 4654
On December 11, 2020, the Food and Drug Administration granted emergency authorization use in the U.S. of the Pfizer/BioNTech COVID-19 vaccine for those 16 years of age and older. Within a week, Moderna was also granted an EAU in the U.S.. Both the Pfizer and Moderna vaccines require two doses, administered a few weeks apart.
Priority allocation of the doses has been given to health care workers and the elderly. It is estimated that it will be spring or summer before the general public will have acess to the vaccines. There are still unanswered questions regarding their safety in pregnant women.
Symptoms and severity
Both seasonal flu viruses (which include influenza A and influenza B viruses) and COVID-19 are contagious viruses that cause respiratory illness.
Typical flu symptoms include fever, cough, sore throat, muscle aches, headaches, runny or stuffy nose, fatigue and, sometimes, vomiting and diarrhea, . Flu symptoms often come on suddenly. Most people who get the flu will recover in less than two weeks. But in some people, the flu causes complications, including pneumonia. The overall hospitalization rate in the U.S. for flu this season is about 69 hospitalizations per 100,000 people, according to the CDC.
With COVID-19, doctors are still trying to understand the full picture of disease symptoms and severity. Reported symptoms in patients have varied from mild to severe, and can include fever, cough and shortness of breath, according to the CDC. Other symptoms may include fever, chills, repeated shaking with chills, muscle pain, headache, sore throat and new loss of taste or smell. COVID-19 symptoms appear to come on more gradually than those of flu, .
Older adults and people with underlying medical conditions, including heart disease, lung disease or diabetes, appear to be at higher risk for more serious complications from COVID-19, compared with people in younger age groups and those without underlying conditions.
The overall hospitalization rate for COVID-19 in the U.S. is about 50 hospitalizations per 100,000 people as of May 8, although the hospitalization rate for adults ages 65 and older is higher, at 162 hospitalizations per 100,000 people, according to the CDC. (However, because fewer people have likely gotten COVID-19 in the U.S. than have gotten the flu, the odds of becoming hospitalized if you have a confirmed case of COVID-19 are thought to be higher than the odds of being hospitalized with influenza.)
Children are a high risk group for complications from flu, but this doesn’t seem to be the case for COVID-19 — few children have been hospitalized with the new coronavirus. A study of published March 18 found that, among 4,226 reported cases, at least 508 people (12%) were hospitalized, and of these, less than 1% were younger than 20 years old.
But recently, COVID-19 has been linked to a rare but serious inflammatory syndrome in children, called pediatric multisystem inflammatory syndrome. New York City has confirmed 100 cases of the syndrome in children, according to .
It’s important to note that, because respiratory viruses cause similar symptoms, it can be difficult to distinguish different respiratory viruses based on symptoms alone, .
Related: Can homemade masks protect you from COVID-19?
Coronavirus science and news
—Coronavirus in the US: Map & cases
—What are coronavirus symptoms?—How long does coronavirus last on surfaces?—Can people spread the coronavirus after they recover?
Which virus makes you sicker?
In the current season, there have been at least 34 million cases of flu in the United States, 350,000 hospitalizations and 20,000 flu deaths, according to the C.D.C. Hospitalization rates among children and young adults this year have been unusually high.
There would be even more illnesses and deaths if there were no flu vaccine. Most people recover in less than two weeks, and sometimes in just days.
By contrast, at least 90,000 people in the United States have been infected with the new coronavirus by late March, and there have been at least 1,400 deaths. There are no treatments or vaccines for the coronavirus, only supportive care for infected people.
Most cases of coronavirus infection are not severe, but some people do become quite sick. Data from the largest study of patients to date, conducted in China, suggests that of coronavirus patients receiving medical attention, 80 percent had mild infections, about 15 percent had severe illnesses, and 5 percent were critical. (But many of the mild infections included patients with pneumonia, experts later learned.)
The first symptoms, fever and cough, are similar to that of the flu, so the diseases can be hard to tell apart without a test to identify the virus. Pneumonia is common among coronavirus patients, even among those whose cases are not severe.
Experts think there may also be many people with no symptoms at all, or such mild ones that they never bother to seek medical attention. Because those cases have not been counted, it’s not possible now to know the real proportion of mild versus severe cases.
The bottom line
COVID-19 and the flu are both respiratory illnesses. While there’s a lot of overlap between them, there are also key differences to look out for.
Many common symptoms of the flu aren’t common in cases of COVID-19. Flu symptoms also develop suddenly while COVID-19 symptoms develop gradually. Additionally, the incubation period for the flu is shorter.
COVID-19 also appears to cause more severe illness compared to the flu, with a larger percentage of people requiring hospitalization. The virus that causes COVID-19, SARS-CoV-2, also seems to transmit more readily in the population.
If you think that you have COVID-19, isolate yourself at home away from other people. Let your doctor know so that they can work to arrange testing. Be sure to keep careful track of your symptoms and seek prompt medical care if they begin to worsen.
On April 21, the FDA approved the use of the first COVID-19 home testing kit. Using the cotton swab provided, people will be able to collect a nasal sample and mail it to a designated laboratory for testing.
The emergency use authorization specifies that the test kit is authorized for use by people who healthcare professionals have identified as having suspected COVID-19.
Similarities: COVID-19 and the Flu
Symptoms
- Both illnesses can cause fever, cough, body aches, and sometimes vomiting and diarrhea (especially in children). Learn more about COVID-19 symptoms.
- Both can result in pneumonia.
- Both flu and COVID-19 can be mild or severe, or even fatal in rare cases.
How It Spreads
- Both the flu and COVID-19 spread in similar ways. Droplets or smaller virus particles from a sick person can transmit the virus to other people nearby. The smallest particles may linger in the air, and another person can inhale them and become infected.
- Or, people can touch a surface with viruses on it, and then transfer the germs to themselves by touching their face.
- People infected with the coronavirus or the flu may not realize they are sick for several days, and during that time can unknowingly spread the disease to others before they even feel sick.
Treatment
- Neither the flu nor COVID-19 is treatable with antibiotics, which only work on bacterial infections.
- Both are treated by addressing symptoms, such as reducing fever. Severe cases may require hospitalization and very ill patients may need a ventilator — a machine that helps them breathe.
- Antiviral medications may shorten the duration of both illnesses.
Myth 2: Lockdowns slow the spread
But let’s pretend for a while that it isn’t better. Because without the fundamental assumption that spreading = bad, the rest of the discussion is flipped on its head. ‘Spikes’ become cause for relief, not concern. Masks, if they work, would become counter-productive. I am not claiming this as truth—only that it is at least as likely as the classical model.
But if you can suspend your disbelief for long enough to imagine that hindering the spread of the virus is worthwhile, then you might be forgiven for assuming that lockdowns are the way to do it. There is, however, no suggestion, let alone evidence, that lockdowns would pose a problem for a wily virus.
Also on rt.com
The problem of false positives from Covid-19 tests means UK is inflating its numbers – and taking wrong decisions
If lockdowns played any part at all, we would expect to see a correlation between the different forms of lockdowns enforced by various regions or countries, and the shape of the death curves there. But we do not—the correlation is zero. Belgium, the UK, New York: strict lockdowns; lots of deaths. Sweden, Japan, Uruguay: light or no lockdowns; few deaths. You can point to opposite examples, but that’s just the point—there is no consistency. And before you try to explain away individual countries with hand waving about ‘different cultures’ or ‘better testing’, there is no correlation with any of those things either.
Simply put, there is nothing that can be easily pointed at to suggest that any measure taken by any government in the world to block the virus has worked. Lockdowns may be the biggest tools in the shed, but they are still faulty.
Myth: Drinking bleach or other disinfectants can protect you from COVID-19
You absolutely should not drink bleach or other household disinfectants, and you should also not spray them on your body. These substances are poisonous if ingested, and they can also cause damage to the skin and eyes, according to the World Health Organization.
When ingested, sodium hypochlorite (household bleach) can cause what is called «liquefactive necrosis,» or a process that results in the transformation of tissue into a liquid viscous mass, Live Science previously reported. The bleach can also damage cells as the sodium reacts with proteins and fats in a person’s tissues in a process called saponification (soap), medical doctors reported in 2018 in a publication by the .
Alarmingly, nearly 4 in 10 American adults in a recent survey reported engaging in dangerous cleaning practices to prevent COVID-19, such as washing food with bleach, using household disinfecting products on their skin or intentionally inhaling vapors from cleaning products, Live Science previously reported.
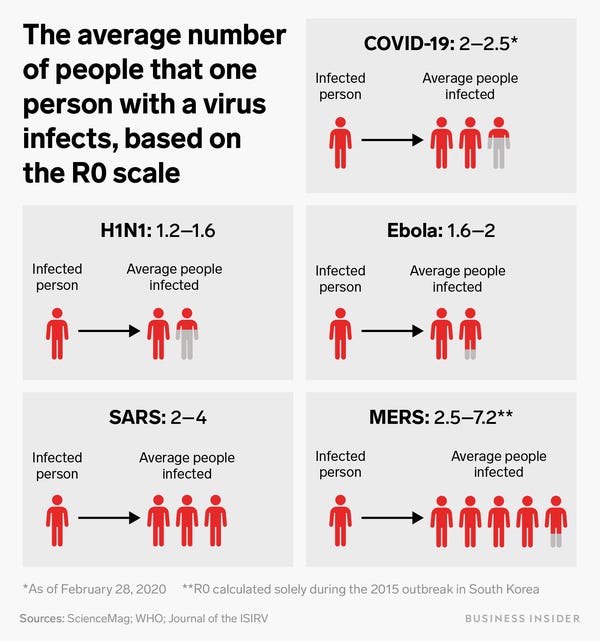
Virus transmission
In both the flu and coronavirus, the main method of transmission appears to be from person to person via respiratory transmission—essentially by coming in close contact (within six feet) with respiratory droplets from the coughs and sneezes of infected people. The flu and coronavirus also have similar periods of time when people are asymptomatic but still contagious. “It appears that with both viruses, people may be able to transmit the virus before they are symptomatic,” explains Dr. Juthani.
However, the latest evidence suggests COVID-19 is much more contagious and spreads more rapidly than the flu.
“In public health we measure something called the R0 (pronounced ‘R-naught’) which is the average number of people infected by a person with the virus,” says Dr. Brown. He goes on to explain that the R0 for influenza is about 1.3, meaning about 1.3 people get the virus from every ten who have the infection. Measles, on the other hand, is extremely contagious, with an R0 of 12-18. (But, of course, we have a measles vaccine.) As for COVID-19? A recent CDC analysis of confirmed cases in China puts the Ro for SARS-CoV-2 at 5.7. That’s up from a previous estimate of 2.2, according to the study, released ahead of its slated publication in the journal Emerging Infectious Diseases.
An R0 of 5.7 means that 82% of the population must be immune to the virus—through vaccination or prior infection—to achieve so-called herd immunity, the study authors note. At 2.2, only 55% of the population would need to be immune to stop transmission.
RELATED: No, Coronavirus Was Not Caused by ‘Bat Soup’–But Here’s What Researchers Think May Be to Blame

A policeman uses a digital thermometer to take a driver’s temperature at a checkpoint at a highway toll gate in Wuhan, China on January 23, 2020.
Chinatopix/AP
China has quarantined Wuhan and 11 other cities to stop the virus’ spread, though cases have been reported in 16 other countries, including the US, France, and Japan.
The outbreak isn’t considered a pandemic, however. The World Health Organization has so far not declared it a global public-health emergency either.
«Familiarity breeds indifference,» Schaffner said. «Because it’s new, it’s mysterious, and comes from an exotic place, the coronavirus creates anxiety.»
Aria Bendix contributed reporting for this story.
Myth: The virus was probably made in a lab
No evidence suggests that the virus is man-made. SARS-CoV-2 closely resembles two other coronaviruses that have triggered outbreaks in recent decades, SARS-CoV and MERS-CoV, and all three viruses seem to have originated in bats. In short, the characteristics of SARS-CoV-2 fall in line with what we know about other naturally occurring coronaviruses that made the jump from animals to people.
A study published March 17 in the journal Nature Medicine also provided strong evidence against the «engineered in a lab» idea. The study found that a key part of SARS-CoV-2, known as the spike protein, would almost certainly have emerged in nature and not as a lab creation, Live Science previously reported. What’s more, if scientists were trying to use computer models to engineer a deadly virus based on the original SARS virus, they likely would not have chosen the mutations that actually appear in SARS-CoV-2. That’s because computer simulations show that mutations in SARS-CoV-2 don’t seem to work very well at helping the virus bind to human cells, Live Science previously reported. But it turns out, nature is smarter than scientists, and the novel coronavirus found a way to mutate that was better — and completely different— from anything scientists could have predicted or created, the study found.
Summary
COVID-19 and flu share some similar symptoms. The symptoms of flu tend to occur faster and can have greater variation. But COVID-19 is more likely to lead to severe illness or death.
Both viruses spread via person to person contact. Flu spreads faster and is more likely to affect children.
As the flu has been around longer, there are several effective antiviral treatments and vaccines available. Researchers and scientists are developing these for COVID-19, but treatments and vaccines are not likely to be available soon.
The best way to prevent COVID-19 is to practice social distancing, which means avoiding any non-essential social contact or travel. It is essential to maintain good personal and domestic hygiene by washing the hands regularly and keeping surfaces and utensils clean.
Viral infections cause both COVID-19 and the flu. But COVID-19 is due to the SARS-CoV-2 virus, and flu is from influenza A and B viruses.
Легкая форма заболевания
После заражения наступает инкубационный период, во время которого вирус вместе с током крови распространяется по организму. Продолжительность этого этапа составляет от недели до двух. Но есть сведения, что, если заражение происходило от одного человека к другому, инкубационный период составляет в среднем 5 суток. По его завершении у инфицированного человека развиваются первые симптомы. До этого момента человек не чувствует себя заболевшим. При легком течении коронавирус чаще всего проявляет себя так:
- повышение температуры до +37…+38°C;
- тошнота;
- кашель без отделения мокроты;
- слабость общего характера;
- повышенная утомляемость;
- заложенность носа;
- диарея;
- сниженный аппетит.
По дням симптомы нарастают – сперва наблюдают слабость и утомляемость, снижение аппетита. На 2-3 сутки приходит гипертермия, заложенность носа и прочие проявления. Их интенсивность нарастает, лекарства помогают слабо, нужна консультация с врачом. Если есть такая симптоматика, при обращении в больницу врачи обязаны выполнить лабораторные анализы на инфекцию и сделать рентген легких. Обычно при легком течении какие-либо структурные изменения отсутствуют. Человека при подобной клинической картине не госпитализируют, он лечится дома. Терапия по большей части направлена на устранение симптомов, выздоровление наступает через 1-2 недели.
Both the flu and the coronavirus can be transmitted from person to person via coughing and other close contact.
Samantha Lee/Business Insider
So far, experts report that the median age of those who have died from the Wuhan coronavirus is around 75. Many of these individuals had other health issues like high blood pressure, diabetes, and Parkinson’s disease.
According to Adrian Hyzler, chief medical officer at Healix International, children, elderly people, pregnant women, and those who are immuno-compromised are more susceptible to the Wuhan coronavirus’ severest complications.
«The people who are likely to die at first will be people who have other illnesses,» he told Business Insider. «But as it spreads, it’ll pick up more people like flu does — people in their 30s, 40s, who are otherwise good and well but unfortunately get ill,» Hyzler’s added. His firm offers risk-management solutions for global travelers.

Health Officials in hazmat suits wait at the gate to check body temperatures of passengers arriving from the city of Wuhan, China, on January 22, 2020, at the airport in Beijing.
Emily Wang/AP
Currently, the fatality rate for the coronavirus is less than 3%. While the flu’s fatality rate is lower than that, the CDC is still far more concerned about protecting Americans from influenza.
Every year, the flu causes between 9.3 million and 49 million illnesses in the US.
«It is currently flu and respiratory disease season, and CDC recommends getting vaccinated, taking everyday preventive actions to stop the spread of germs, and taking flu antivirals if prescribed,» the agency said in a statement Friday.
How R0 works
A given pathogen’s R0 value changes with place and time.
«There is no R0 — there is an R0 in a population,» Elizabeth Halloran, a biostatistician at Fred Hutchinson Cancer Research Center and University of Washington, told Business Insider. A recent CDC study found that the coronavirus’s R0 was as high as 5.7 in the early days of its Wuhan outbreak.
An R0 value of 1 means the average person who gets that disease will transmit it to one other person; in that case, the disease is spreading at a stable rate. An R0 of more than 1 means the disease spreads exponentially.
When experts strategize about how to end the pandemic, their goal is to bring the R0 below 1, which would put the coronavirus in decline until it dies out.
Shayanne Gal/Business Insider
Controlling one key factor — social interaction — is crucial in lowering the R0 of any disease.
«Even measles, if it’s out in the country, doesn’t have a very high R0 because you have to interact with a certain number of people to be able to infect them,» Halloran said. «Part of the transmission involves social contacts between people, and the R0 depends on how fast people are interacting with each other.»
Differences: COVID-19 and the Flu
Cause
COVID-19: Caused by the 2019 coronavirus, also known as SARS-CoV-2.
Flu: Caused by any of several different types and strains of influenza viruses. Different strains circulate each year.
Symptoms
COVID-19: Many people infected with the coronavirus do not feel sick or have any symptoms at all, but they can still transmit the coronavirus to other people. Review the full list of symptoms.
Unlike the flu, COVID-19 can sometimes cause a person to suddenly lose their sense of smell (anosmia) or taste (ageusia).
Flu: Flu does not typically affect a person’s sense of smell or taste.
Treatment
COVID-19: Antiviral medications and other therapies are being tested to see if they can effectively address symptoms and shorten the duration of the illness. Currently, effective treatments are only available in an intravenous form, so they are not prescribed to patients outside of a hospital setting.
Flu: Oral antiviral medications can address symptoms and sometimes shorten the duration of the illness. Because they are given by mouth, these antiviral therapies can be prescribed for patients who are not hospitalized as well as for those in the hospital.
Vaccine
COVID-19: No vaccine is available at this time, though development and testing are in progress.
Flu: A vaccine is available and effective in preventing some of the most dangerous types or to reduce the severity or duration of the flu. It is very important to get vaccinated for the flu this year.
Myth: Wearing masks can cause CO2 poisoning
Wearing medical masks for long periods may be uncomfortable for some, but it does not cause oxygen deficiency or carbon dioxide (CO2) intoxication (when too much CO2 builds up in the bloodstream), according to WHO. The same applies for N95 masks and cloth face coverings, according to .
«Rebreathing tiny amounts of CO2 from wearing either properly fitted N95 respirators or more loosely fitted cloth or surgical masks is of no concern for the vast, vast majority of people,» Darrell Spurlock Jr., the director of the Leadership Center for Nursing Education Research at Widener University in Pennsylvania, told Healthline. «The ‘dose’ of CO2 we might rebreathe while masking is quickly and easily eliminated by both the respiratory and metabolic systems in the body.»
When you wear a mask, you should make sure it has a snug fit but allows you to breathe normally, WHO says.
Editor’s Note: This story has been updated to reflected updated knowledge on SARS-CoV-2 transmission in children.
Tia Ghose, Yasemin Saplakoglu, Nicoletta Lanese, Rachael Rettner and Jeanna Bryner contributed to this article.
Originally published on Live Science.
With impressive cutaway illustrations that show how things function, and mindblowing photography of the world’s most inspiring spectacles, represents the pinnacle of engaging, factual fun for a mainstream audience keen to keep up with the latest tech and the most impressive phenomena on the planet and beyond. Written and presented in a style that makes even the most complex subjects interesting and easy to understand, is enjoyed by readers of all ages.



